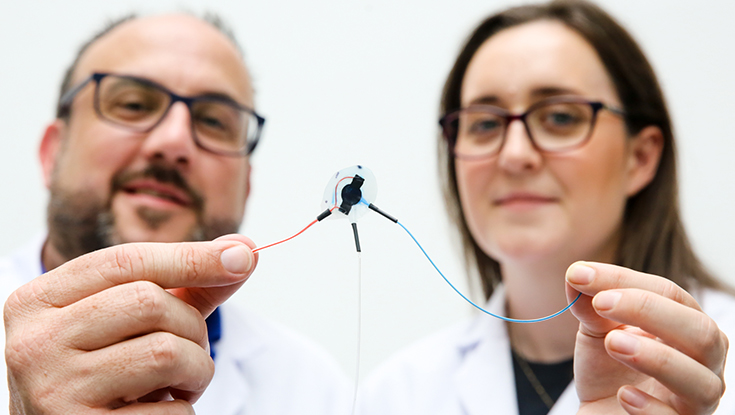
Scientists at the University of Galway in Ireland and MIT have collaborated to create a soft robotic implant that can work to fight fibrotic encapsulation and deliver drugs despite the presence of fibrous scar tissue. The device, which the researchers have termed the FibroSensing Dynamic Soft Reservoir (FSDSR), is designed to reside in the body for extended periods and deliver drugs. However, the immune system typically recognizes such medical implants as foreign, and walls them off with a thick layer of fibrous scar tissue, limiting drug diffusion and leading to eventual failure. This new soft robotic implant can inflate and deflate, like a sea creature, which helps to reduce the amount of scar tissue that is deposited on its surface. However, in a key development, the researchers have also furnished the implant with a sensor that can measure the amount of scar tissue present on the device, allowing it to use “AI” to calculate how to release the same dose of drug, regardless of the amount of fibrosis present.
The foreign body response is a key hurdle in developing more effective medical implants, such as an artificial pancreas. The thick scar tissue that builds up on such implants greatly reduces their lifespan and limits their ability to sense their environment and release drugs in response. Techniques to reduce this biofouling, such as surface patterning on medical implants, have met with mixed success.
To address this, these researchers have created a soft robotic drug delivery implant that can reduce the foreign body response by actively inflating and deflating. This movement appears to confuse the body, which can’t deposit as much scar tissue on the device. This robotic actuation also serves another purpose, by helping to push liquid drug out of the device into its surroundings. So far, so good, but in this latest study, the researchers took it a step further by introducing “artificial intelligence,” according to a press release from the University of Galway.
They incorporated a sensor membrane into the device that can sense the amount of biofouling that has occurred. Then, machine learning calculates how many actuations, and of what force, the device will need to apply to squeeze a consistent dose of drug through the surrounding fibrous capsule. In this way, the technology can continue to deliver consistent drug dosing even if it is heavily covered in fibrotic scar tissue. The technology may pave the way for fully autonomous implants that can monitor their environment and make adjustments as required to achieve their goals.
“This is a new area of research that can have implications in other places and is not solely limited for the treatment of diabetes,” said Garry Duffy, a researcher involved in the study. “Our discovery could provide consistent and responsive dosing over long periods, without clinician involvement, enhancing efficacy and reducing the need for device replacement because of fibrosis.”
Study in journal Science Robotics: Soft robot–mediated autonomous adaptation to fibrotic capsule formation for improved drug delivery
Via: University of Galway